Airway Emergencies
In some cases, the anesthesia care provider can predict a difficult airway; in other cases, it can be unexpected. The perioperative nurse must be prepared to provide extra assistance in both circumstances. It is important to know exactly where all pieces of airway equipment are located including the difficult-airway cart.
If the patient is known to be a difficult airway, the difficult intubation cart, as well as other intubation assistive devices, should be in the room and ready for use before the patient arrives.
If an airway emergency occurs unexpectedly, the perioperative nurse should alert others and stay at the bedside to assist the anesthesia care provider. Additional help can bring the difficult airway cart and any other necessary supplies.
🧩 Practice Activity: Predictors of a Difficult Airway
Choose one or multiple responses to answer the question. Select “Check” when you feel confident in your answer.
Unanticipated Airway Emergencies
Sometimes a patient experiences an airway emergency during induction or extubation. Perioperative personnel must always anticipate that an airway emergency can occur, including laryngospasm and bronchospasm.
Unanticipated Airway Emergencies: Laryngospasm
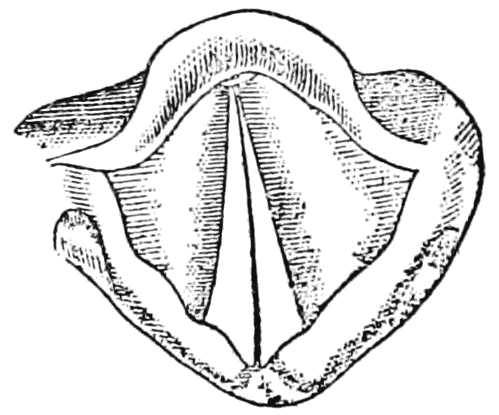
What is a laryngospasm?
- Closure of the vocal cords where the larynx closes the glottis by contracting.
- It is the body’s natural response to prevent substances from entering the lungs.
- If a complete obstruction occurs, the patient may experience hypoxia, no audible air entry, and bradycardia.

Who is at Risk for Laryngospasm?
Elevated risk patients include:
- Children under the age of 9, with the highest risk between 1-3 months of age.
- Patients with Down Syndrome because of a large tongue and increased secretions.
The risk is also increased if the patient has had a recent respiratory tract infection since airway irritability can last 4-6 weeks post infection. It’s also a risk if the patient was intubated with an endotracheal tube which causes irritation.
(Karsli et al, 2002)
Managing a Laryngospasm
Mild Episode
Severe Episode
(Karsli et al, 2002)
Unanticipated Airway Emergencies: Bronchospasm
What is a Bronchospasm?
Bronchospasm is a lower airway obstruction caused by spasm within the bronchioles. Because the bronchioles do not have strong cartilage supports, these spasms can cause a complete collapse and airway closure.
What Causes Bronchospasm?
There are many varied factors that can contribute to bronchospasm in perioperative patients. Some key factors to consider include:
- Anesthesia in a poorly controlled asthmatic.
- Bronchial intubation.
- Irritation of carina from tracheal tube and/or aspiration of gastric contents.
- Use of irritant volatile anesthetic drugs.
- Intubation without use of a relaxant at an inadequate depth of anesthesia.
- Allergic response to medication being given.
(Odom-Forren, 2019)
Managing a Bronchospasm
(Odom-Forren, 2019)
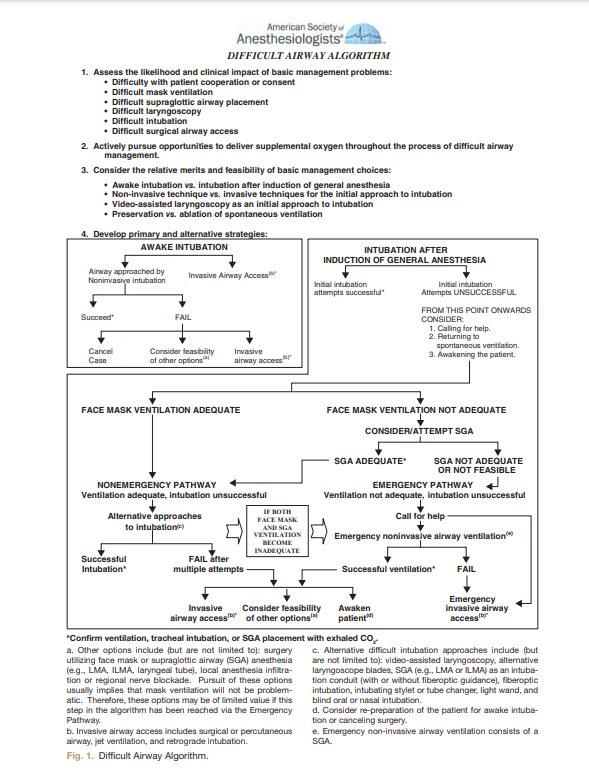
Managing a Difficult Airway
The most crucial step when there is a known difficult airway, is to COMMUNICATE.
Before the patient enters the room, the perioperative team should discuss the plan of care, which items are needed and what additional assistance may be required.
Ensure that the surgical briefing includes a review of all equipment and steps the team is planning to take. Assign a lead, usually the anesthesia care provider, as well as hands free personnel who can assist or grab items as needed.
Other common considerations when there is a known difficult airway:
Pre-oxygenation of the patient is vital. This should be done with a tight-fitting face mask. Pre-oxygenation can also be used as a strategy with difficult airways. This means having a nasal cannula in the nares providing passive oxygen delivery while attempting to intubate.
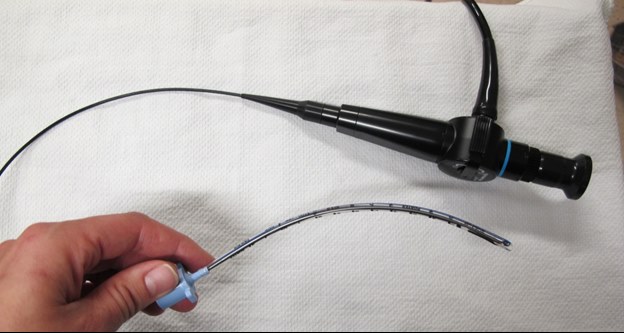
Use technology such as video laryngoscope, fiberoptic bronchoscope or glidescope to assist with visualization. This is to help limit the number of attempts at intubation which can cause trauma and increase the risk of hypoxemia or aspiration.
If difficulties continue and it is not possible to intubate the patient, consider alternatives that allow for ventilation:
- Supraglottic airway device (LMA)
- Cancelling the case and maintaining the airway with mask ventilation until the patient wakes up
- Last resort – Emergency tracheostomy
- Awake fiberoptic intubation using local freezing may be required
(Asai, 2018)
Watch this video to see patient information on awake intubation:

Difficult Airway Cart/Container
The World Health Organization has recommended that ALL surgical centres have an emergency airway container or cart that is available within 60 seconds. All the equipment must be:
- Compatible
- Restocked and secured after every use
The location of the cart/container must be known to all perioperative personnel.
Contents of the Difficult Airway Cart/Container
It is not necessary for perioperative nurses to memorize what is in the difficult airway cart; however, all perioperative nurses must be aware of the contents and be able to obtain and navigate it in emergencies. The World Health Organization recommends that all difficult airway carts include:
- Short laryngoscope handle
- At least one alternative blade
- Intubating LMA (#3,4,5) with fast-track tubes
- Specialized tracheal tubes
- Flexible intubating bronchoscopes with battery light source
- Fiber-optic equipment (airways, local anesthetic spray, bite block, etc.)
- Surgical cricothyroidotomy kit
- Pulse oximeter
- Oesophageal intubation detector (capnograph)
(WHO, 2009)